Early Recognition is Key for a Successful Outcome
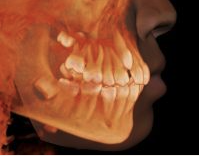
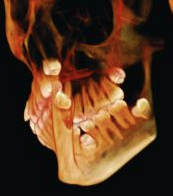
The American Association of Orthodontists recommends that growing patients should be evaluated to determine potential problems with erupting adult teeth. A panorex screening x-ray can be used to determine if all adult teeth are present and whether any unusual areas could block the eruption of a permanent tooth.
Other factors that might affect the eruption of a permanent tooth include limited space in the jaw and overcrowding. Typically, a general dentist completes this screening, and then a referral is given to visit an orthodontist to open the space for proper tooth eruption.
A general dentist might also refer Naperville patients to see an oral surgeon if a tooth extraction is needed. Extra teeth can be removed, as well as growths that are blocking the eruption of adult teeth. When the eruption path is cleared at an early age, it increases the likelihood that the impacted tooth will erupt naturally. The older the patient is, the higher the likelihood that the tooth is fused in position. Even if the dental arch space is available for the tooth to grow in, impacted teeth don’t always erupt without treatment. At this point, recommended treatments are usually focused on the extraction of the impacted tooth and replacement using a dental implant or fixed bridge.